Conditions
Conditions that cause shoulder pain.
Definition:
Painful, stiff shoulder due to inflammation and tightening of the ligaments connecting the bones of the shoulder.
Symptoms:
Severe pain and limitations in range of motion, particularly reaching behind the back. Patients typically have maintained strength but severe fleeting pain with sudden movements.
Non-Operative Treatment:
Anti-inflammatory pills, cortisone injections, and specific physical therapy.
Operative Treatment:
Arthroscopic release of the tight ligaments.
Recovery:
Physical therapy 5 times a week for 3 weeks to maintain the range of motion.
Details:
When the ligaments are too loose, the shoulder is unstable and often dislocates. When the ligaments are too tight, the shoulder is painful and stiff. This condition is called Adhesive Capsulitis or frozen shoulder. Frozen shoulder is particularly common in women between the ages of 40 and 60. The risk factors that can lead to Adhesive Capsulitis include diabetes and thyroid disorders. Only 40% of cases are the result of a traumatic event. The majority of painful stiff shoulders occur spontaneously. It is common for a patient to have impingement syndrome or bursitis to then develop Adhesive Capsulitis after several weeks.
People with frozen shoulder initially present with severe pain and the loss of motion, particularly reaching behind the back. Patients typically have maintained strength but experience severe fleeting pain with sudden movements. Sleep is usually very painful and restless in this early stage. In this initial stage, called the freezing stage, the treatment revolves around pain control. Slings can be used for comfort but are discouraged because they can lead to more stiffness and pain. The second stage is the frozen stage which is heralded by the lack of pain. During this stage, patients are often happy as their shoulder is no longer painful. The range of motion is not improved in the frozen stage. Treatment for this stage centers on cortisone injections, short term courses of prednisone, and specific physical therapy. Eventually, the thawing phase, the final stage of frozen shoulder, is reached. During this stage, the range of motion improves and the pain continues to dissipate. The entire process of Adhesive Capsulitis can last 9-12 months. For patients who do not improve, a shoulder arthroscopy can reclaim the range of motion and diminish pain.
Click Here for a specific video on this topic.
Definition:
The loss of cartilage from the surface of the bones causing inflammation and pain.
Symptoms:
Pain and stiffness.
Non-Operative Treatment:
Anti-inflammatory pills, physical therapy, and cortisone injections.
Operative Treatment:
Arthroscopic removal of bone spurs and removal of the end of the clavicle when the arthritis involves the acromioclavicular joint. Total shoulder replacement when the arthritis involves the glenohumeral joint.
Recovery:
Sling for a couple days for the arthroscopic treatment. Sling for 3 weeks after a shoulder replacement.
Details:
Arthrosis is defined as the loss of articular cartilage. When this condition is accompanied by inflammation it is known as arthritis. Arthrosis may not hurt, but arthritis with the inflammation invariably does cause pain. Arthrosis is very commonly seen about the acromioclavicular (AC) joint and arthritis presents with pain at the top of the shoulder that can be reproduced by manual palpation. As the cartilage wears away, the bones with their exposed nerve fibers rub against each other causing inflammation and pain. See Figure 1.
People with AC joint arthritis will often have their symptoms reproduced with pressure over the AC joint and when they reach across their bodies, such as when they try to touch the other shoulder. The treatment for symptomatic AC joint arthritis usually centers around behavior modification (if it hurts when you do something, don’t do it!), anti-inflammatory medications, cortisone injections, and surgery. The medications and the injections are meant to decrease the inflammation of the arthritis and turn it into an arthrosis which hopefully will not hurt.
Because the exposed bones still rub against each other, the pain may recur necessitating surgery to fix the problem. Because this joint has very little motion, surgery consists of excising the final 8-10mm of the clavicle. See Figure 2. See video of End of Clavicle Excision.
More commonly, people will have x-ray evidence of AC joint arthrosis but have no pain over the AC joint. These people often have other causes of their pain such as impingement syndrome or capsulitis.
Arthrosis of the glenohumeral joint is a much more serious entity. This condition is defined by the loss of remaining articular cartilage on the humeral head and glenoid. See Figure 3 & 4.
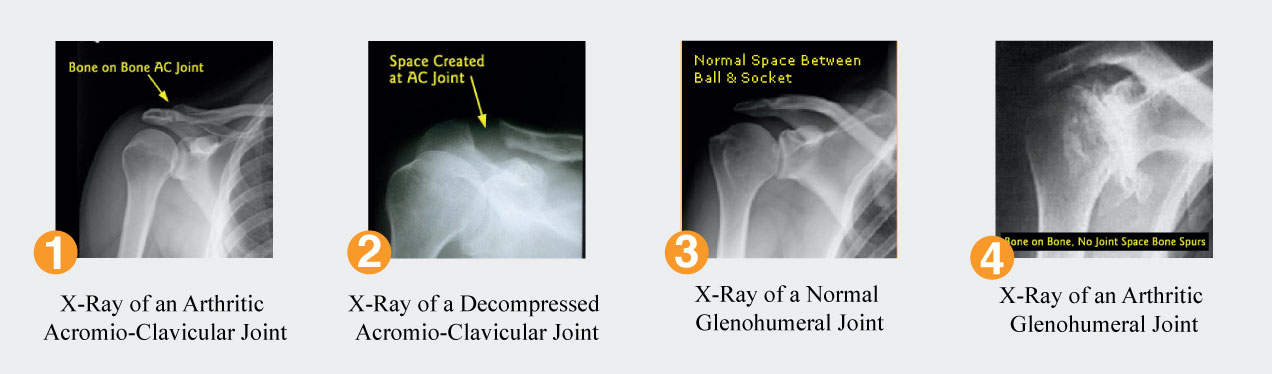
Characterized by stiffness and a crunching sensation, glenohumeral arthrosis will evolve into arthritis with the onset of inflammation and pain. Unlike AC joint arthritis, physical therapy is helpful with glenohumeral arthritis as it can improve the flexibility of the joint thereby decreasing joint reactive forces and allowing parts of the joint with remaining articular cartilage to move against each other. Anti-inflammatory medications and cortisone injections are designed to decrease the inflammation (thereby decreasing the pain) which can facilitate the efforts of the physical therapists.
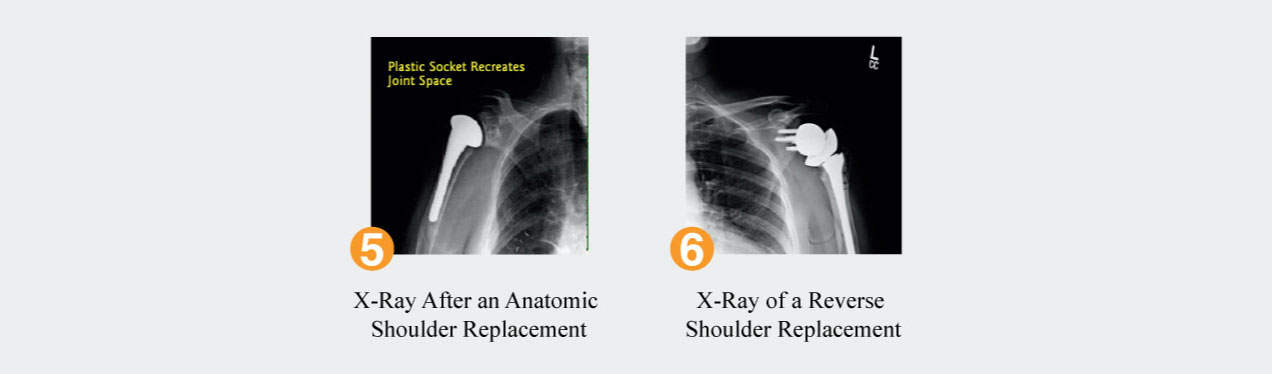
Surgery for glenohumeral arthritis is reserved for those cases when the pain is not controlled by the above non operative treatments. The most reliable surgery is a replacement of the top of the humerus by a metal ball and a replacement of the glenoid by a polyethylene medical grade plastic socket. This surgery has been shown to give long term pain relief with improved function. Known as a total shoulder replacement, this surgery is very reliable but its success depends on a well functioning rotator cuff. See Figure 5.
In properly selected patients, those with low demands on their shoulder, a shoulder replacement has been shown to last for fifteen or more years. Recently, new advances have allowed surgeons to reproduce the exact anatomy of the patient’s own shoulder allowing the shoulder replacements to last even longer.
When the rotator cuff is either torn or not functional in the setting of glenohumeral arthritis, a special shoulder replacement is used called a reverse shoulder replacement. This involves reversing the position of the ball and socket and places the ball on the glenoid and the plastic socket on the humeral side. See Figure 6.
Visit our YouTube channel for specific videos on this topic.
Definition:
Tear or inflammation along the course of the biceps tendon.
Symptoms:
Pain running down the front of the shoulder along the biceps.
Non-Operative Treatment:
Physical therapy and cortisone injections are very successful.
Operative Treatment:
Biceps tenotomy and tenodesis are effective in reducing the pain and maintaining the function and strength of the biceps.
Recovery:
The recovery from a biceps tenodesis is very quick but is often performed in conjunction with a rotator cuff repair which in of itself tends to have a long recovery.
Details:
The biceps tendon which runs up the arm has two parts, a long head and a short head. The long head of the biceps inserts onto the top of the glenoid and blends in with the labrum which is the cartilage that surrounds the glenoid. The short head attaches to the coracoid process. The long head is a common cause of shoulder pain as it runs in a tunnel called the intertubercular groove. The long head of the biceps is prone to tendonitis as it runs through this groove and it is prone to tears.
The biceps also is intimately related to SLAP tears as it attaches to the superior labrum. Many patients with SLAP tears will also have pain down their biceps muscle. The initial treatment for people with biceps tears is physical therapy and, frequently, a cortisone injection can be helpful. When these treatments fail, a biceps tenodesis can be considered. In this procedure, the long head of the biceps is cut from its insertion on the top of the glenoid and is reattached to the humerus below the shoulder joint. This procedure is effective in alleviating the pain associated with biceps tendonitis and tears and does not weaken the function of the arm.
Click Here for a specific video on this topic.
Definition:
Bursitis is inflammation of the bursa that lies between the acromion and the rotator cuff tendon. Bursitis is often caused by impingement of a hooked acromial bone spur onto the bursa. Inflammation of the rotator cuff tendons is called rotator cuff tendinitis. Rotator cuff tears occur when the tendon is detached off the bone.
Symptoms:
Pain along the side of the shoulder aggravated by reaching overhead or behind and by sleeping on the shoulder. Tears have the same symptoms as well as weakness.
Non-Operative Treatment:
Physical therapy and cortisone injections.
Operative Treatment:
Arthroscopic removal of the inflamed bursa and the hook on the undersurface of the acromion. For rotator cuff tears, the only treatment that will re-attach the tendon to the bone is surgery.
Recovery:
Sling is worn for a few days for comfort only. The sling stays on for 3-6 weeks after rotator cuff repair surgery depending on the size of the tear.
Details:
The rotator cuff is comprised of four muscles that come off the scapula. These four muscles are the subscapularis, infraspinatus, and teres minor and supraspinatus. Each muscle is attached to the top of the humerus by a tendon. The tendons run under prominences on the scapula called the acromion and the coracoid.
Each of these bony processes can be particularly prominent and rub against the underlying tendons. The acromion rubs against the supraspinatus and the coracoid impinges upon the subscapularis. This is called impingement syndrome and can present with similar symptoms as bursitis. A special tissue called bursa is designed to minimize the irritation between the bone and the tendon. Bursa is a very thin and slippery tissue that has many nerve fibers. The bursa can become inflamed and thickened when it is entrapped between the bone and tendon. Patients with impingement syndrome or bursitis from the acromion on the supraspinatus tendon will notice they have pain with repetitive overhead lifting and reaching behind their bodies to put a coat on or to put money in the toll both. Many patients also complain of pain when they sleep on their affected shoulder. The pain is often localized on the side of the upper arm and the top of the shoulder or even the back of the shoulder.
Impingement of the acromion on the supraspinatus tendon is more common than impingement of the coracoid on the subscapularis tendon. This subcoracoid impingement will present with pain in the front of the shoulder.
The treatment of impingement syndrome and bursitis is very similar regardless of whether it is emanating from the subacromial space or subcoracoid space. Physical therapy is a hallmark of non operative treatment and emphasizes stretching the muscles in the front of the shoulder and strengthening the muscles in the back. Often, the muscles in the front (the pectoralis, the biceps, the anterior deltoid, and the conjoined musculature) are very strong and tight in people. Since these muscles attach to the front of the scapula, they tend to pull the scapula and its accompanying acromion and coracoid down. This worsens impingement. By balancing the muscles of the scapula and strengthening the lower trapezius, the rhomboids, and the serratus anterior (bringing the scapula into a more military position), the scapula can be rotated back and the accompanying acromion and coracoid can be lifted off the rotator cuff tendons.
Anti-inflammatory treatment is also used to decrease the pain from impingement and bursitis. Typically, patients will start with Non Steroidal Anti-Inflammatories (NSAIDs) such as ibuprofen or naproxen. If unsuccessful, a cortisone injection is often tried. When non-operative treatment fails, the treatment of choice is an arthroscopic removal of the inflamed bursa and removal of any bone spurs impinging on the rotator cuff. The recovery of this procedure is rather quick, with most patients out of a sling in a few days and allowed unrestricted range of motion immediately. Most people have enough pain relief to start strengthening exercises within 4-6 weeks after surgery.
When the impingement advances to the point that the rotator cuff tendon tears or if a traumatic episode causes the tendon to tear, the shoulder becomes painful and weak. Patients with small tears will notice that they have difficulty lifting heavy objects and patients with larger tears will have pain lifting up their arm. Pain with sleeping is a frequent complaint of people with rotator cuff tears.
Rotator cuff tears (when completely detached off the bone) do not heal. The tendon retracts and the muscle starts to atrophy. Over time, the tear will get larger and the tendon will become irreparable. As the tear becomes very large, affecting the other rotator cuff tendons, arthritis develops. Because of this bleak scenario, many take an aggressive approach and repair tears in young people. It is certainly possible to treat very small tears with therapy and have the pain diminish, but many prefer to use this approach on people who are not great surgical candidates for medical reasons or if the patient is elderly. Patients under the age of 50 will be advised about the benefit of repairing even small tears because the last thing many want is to explain why they have end stage arthritis at the age of 60.
Visit our YouTube channel for specific videos on this topic.
Definition:
Accumulation of calcium within the rotator cuff tendon causing pain.
Symptoms:
Severe pain along the top and side of the shoulder, often causing people to seek treatment in the emergency room.
Non-Operative Treatment:
Cortisone injections to try to break up the calcium and decrease the accompanying inflammation.
Operative Treatment:
Arthroscopic removal of the calcium deposit.
Recovery:
Sling for a few days unless the rotator cuff needs to be repaired.
Details:
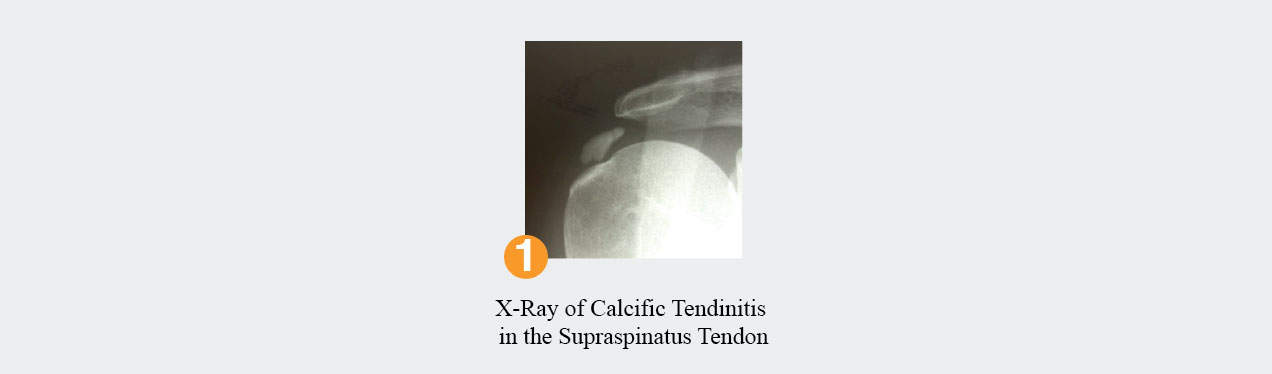
In some cases, calcium crystals will form and coalesce in the rotator cuff tendon. It is not known why this happens, but it is not caused by an increase in calcium intake. Thought to be a degenerative process within the tendon, this condition, like many about the shoulder, is more common the older we get. The condition is diagnosed on x-ray and presents the same way as impingement syndrome but is often worse. View Figure 1. Many cases of calcific tendinitis are so painful that patients have to go to the emergency department for pain relief. The condition can be readily ameliorated by a cortisone injection in the vicinity of and into the calcium deposit. Occasionally, the non-operative treatment of calcific tendinitis fails and arthroscopy is necessary to decompress the collection.
Visit our YouTube channel for a specific video on this topic.
Definition:
A break is the same as a fracture. The bone becomes broken due to trauma and, on rare occasions, from neoplasms.
Symptoms:
Pain that is often accompanied by swelling and ecchymosis (black and blue bruising).
Non-Operative Treatment:
If the bones are fractured (broken) but are still well aligned, then rest in a sling for 4-6 weeks is often successful in facilitating healing.
Operative Treatment:
Surgery is the treatment of choice if the fracture is severe enough that the bones are displaced or if the bones do not heal after 4-6 weeks.
Recovery:
Fractures treated non-operatively can heal in a sling over 4-6 weeks. Physical therapy often starts at 3 weeks with passive range of motion and active range of motion starts at 6 weeks when there is healing of the bone. Most fractures treated with surgery are also started with passive range of motion at 3 weeks and active range of motion at 6 weeks. Maximal function occurs in 3-6 months in most cases.
Details:
Some of the most common fractures about the shoulder involve the top of the humerus where the rotator cuff tendons insert. When the bones are displaced more than 5mm, the mechanics of the rotator cuff may be altered enough that pain develops. Often, surgeons will fix fractures about the top of the humerus in an effort to restore the anatomy of the rotator cuff tendons.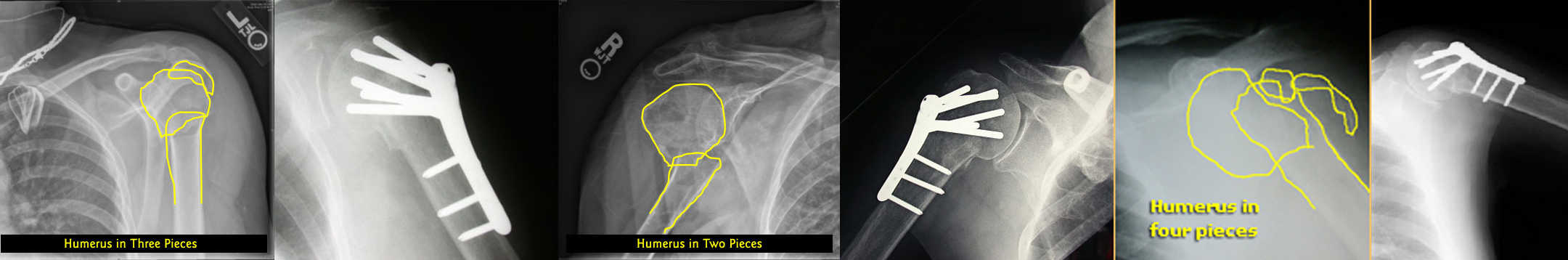
Clavicle
The clavicle is the most commonly fractured bone in the shoulder. Clavicle fractures usually heal and rarely need surgery. It is uncommon to operate on a child with a clavicle fracture, as they invariably heal and remodel. In adults, clavicle fractures may be severe and can necessitate surgery if the bones are broken into several pieces or if the fracture ends are significantly displaced.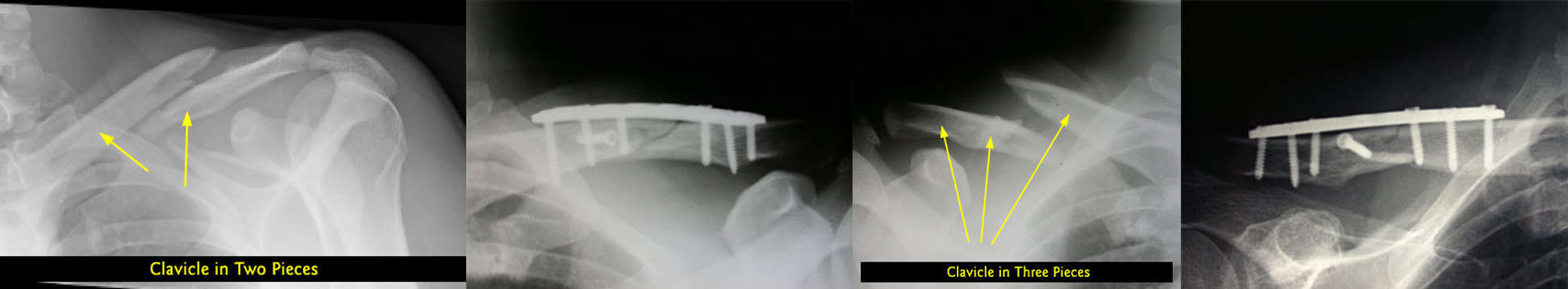
Visit our YouTube channel for a specific video on this topic.
Definition:
A loose or painful shoulder due to stretched ligaments or detachment of the labrum from the glenoid.
Symptoms:
When the stretched ligaments or labral tear is towards the bottom of the socket, people will have a loose shoulder. When the labral tear is at the top of the socket, people will have pain with overhead activities.
Non-Operative Treatment:
Physical therapy.
Operative Treatment:
Arthroscopic repair of the stretched ligaments and torn labrum. A Latarjet procedure is performed in cases of recurrent instability or when there is significant bone damage.
Recovery:
Sling for the first month, especially during sleep when the arm tends to move in awkward positions.
Details:
The shoulder joint between the humerus and glenoid is a confined space surrounded by the capsule which is a thin layer of tissue. The ligaments are thickenings in the capsule and help provide stability to the joint. The ligaments originate from the top of the humerus and insert on the labrum, which is a type of cartilage that surrounds the glenoid. View Figure 1. When the ligaments are stretched, as can be seen in young flexible people, the shoulder may be loose and patients complain that their shoulders move out of the socket. This is called a shoulder subluxation. Sometimes, after a traumatic dislocation the labrum tears off the bone. Since the ligaments attach to the labrum, a torn labrum renders the ligaments ineffective and the patient also may complain of shoulder instability and have the shoulder dislocate out of the socket multiple times.
The treatment of shoulder dislocations is usually surgery in the very young patient because the shoulder will typically continue to dislocate. As the shoulder dislocates, the articular cartilage in the glenohumeral joint can be damaged, predisposing the patient to arthritis.
When there is significant bone damage from repetitive dislocations (called Hill-Sachs and Bankart lesions) it may be necessary to reconstruct the bone of the shoulder. Often, the coracoids is cut and transferred from the scapula and fixed to the glenoid socket. This is called a Latarjet procedure.
In patients over 40, non-operative treatment is often effective because the healing potential of the ligaments is greater (we scar more as we age due to an increase in the stiffness in our ligaments and tendons). In patients over 60, dislocated shoulders often cause rotator cuff tears and the treatment is directed to the rotator cuff.
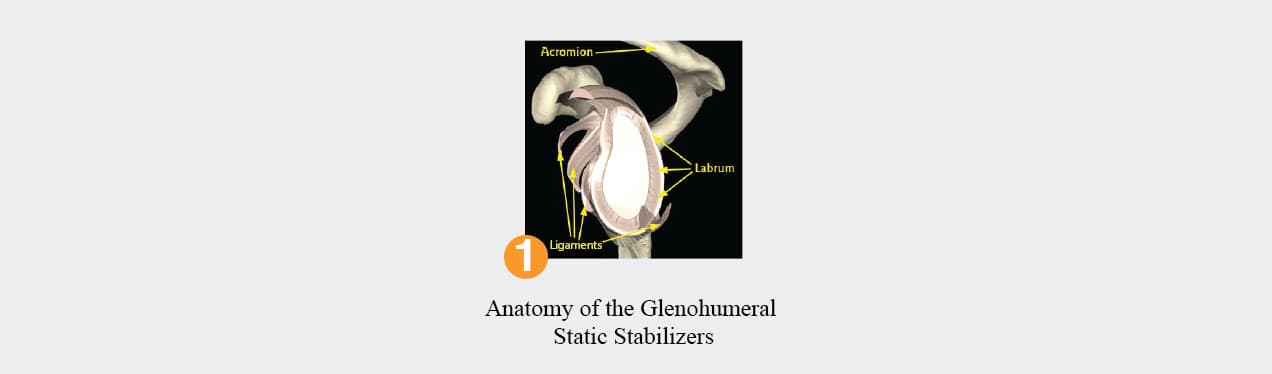
Sometimes the labrum tears and the shoulder is not unstable. These labral tears may cause pain with overhead activities such as throwing or lifting luggage above the shoulder. The superior labrum is commonly detached in patients and is a well known cause of shoulder pain. Because the biceps tendon inserts onto the superior labrum, people with these labral tears may also have pain radiating down their biceps. The treatment is usually to fix the labral tear back to the bone. An acronym used is SLAP, which stands for Superior Labrum Anterior to Posterior. View Figure 2 – 5.
Visit our YouTube channel for videos on this topic.
The other joint about the shoulder, the acromioclavicular (AC) joint, also has ligaments. These ligaments are often injured by an impact onto the top of the shoulder. A separated shoulder is defined as an injury to the ligaments about the AC joint. When the ligament damaged is mild (Types I, II, or III), most prefer to treat these injuries without surgery as most people end up with pain-free, normal shoulder function (although they may have a small bump on the top of their shoulder). Unfortunately, the only way to fix the bump is to operate and that leaves a scar. For severe AC joint separations (Types IV, V, and VI), surgery is often needed to reconstruct the AC joint.
Rotator Cuff Arthropathy and the Reverse Shoulder Replacement
Definition:
Arthritis caused by a large rotator cuff tear.
Symptoms:
Pain and loss of active motion about the shoulder.
Non-Operative Treatment:
Physical therapy and occasional cortisone injections.
Operative Treatment:
Arthroscopic debridement cartilage debris removal of the shoulder in patients with good range of motion and a reverse shoulder replacement in patients with pain and limited range of motion.
Recovery:
A sling for a few days after the debridement and for 3 weeks after the reverse shoulder replacement.
Details:
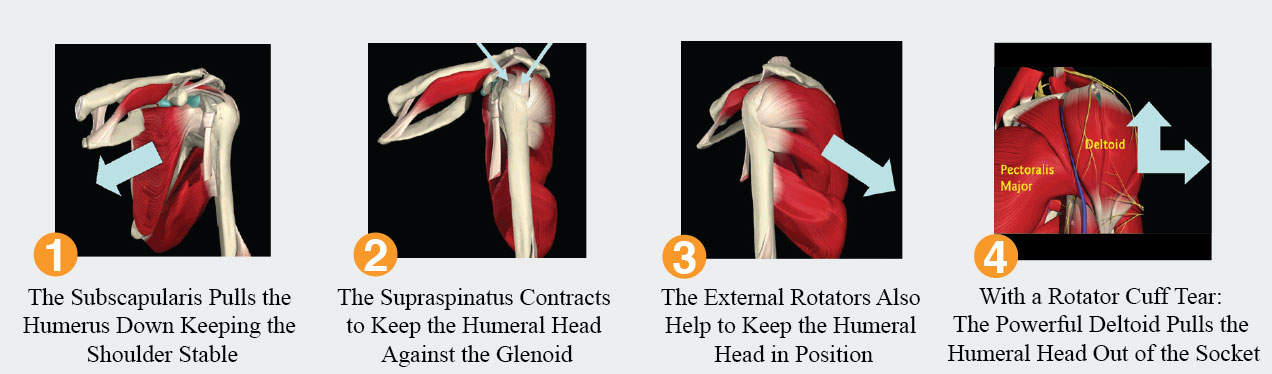
The rotator cuff’s main function is to keep the humeral head centered on the glenoid. Its secondary function is to rotate the humeral head view.
Figure 1 shows how the subscapularis contracts and pulls the humerus down, preventing it from riding high when the deltoid elevates the arm; Figure 2 shows how the supraspinatus contracts and pulls the humeral head into the glenoid socket, preventing the humerus from riding high when the deltoid elevates the arm; Figure 3 shows how the posterior two rotator cuff muscles contract and keep the humerus down and centered on the glenoid, while the powerful deltoid elevates the arm.)
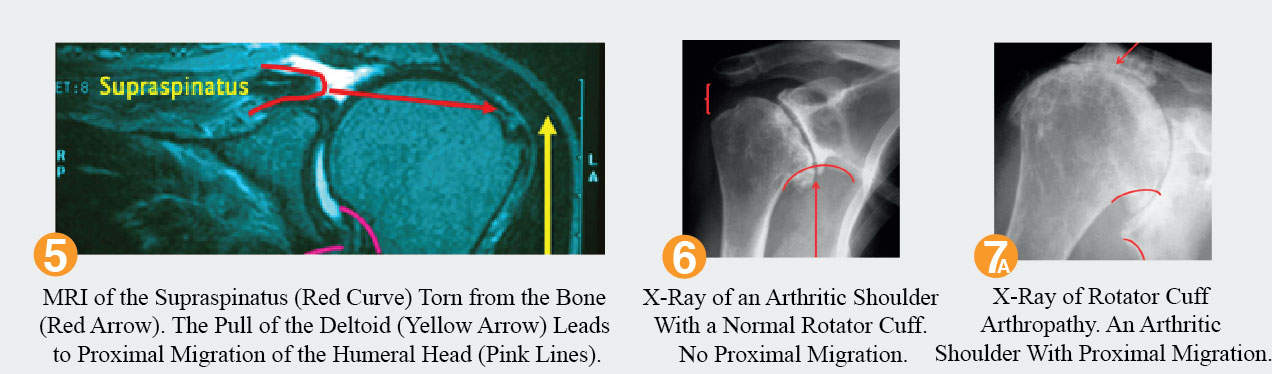
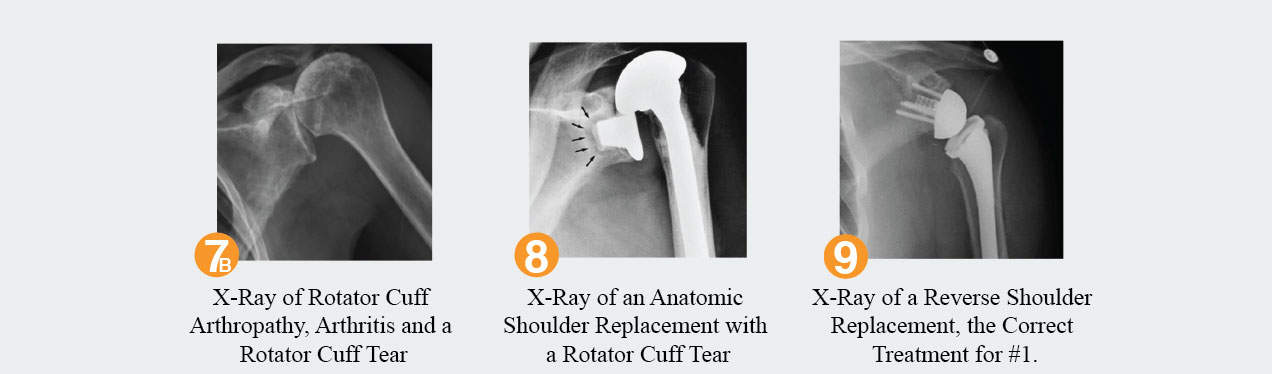
When the rotator cuff is significantly torn, the humeral head will sit high with respect to the glenoid and lead to arthritis. The deltoid causes the humeral head to rise on the glenoid. Figure 4, which depicts the deltoid, a powerful muscle that elevates and abducts the arm; Figure 5 shows an MRI where the rotator cuff is torn causing proximal migration. The supraspinatus is outlined in red and should be attached to the greater tuberosity. The yellow line shows the upward force applied to the humerus by the deltoid and the pink shows the elevation of the humeral head with respect to the glenoid.
Rotator cuff arthropathy is a very difficult problem for any doctor to treat. It is considered an unsolved problem in the young patient who is under 65 years of age. Patients usually present with pain and difficulty lifting their arms. Many of the patients have had rotator cuff repairs that failed and re-tore.
Because rotator cuff tears are essentially the only problem about the shoulder that can lead to such a difficult problem to fix, most shoulder surgeons recommend surgery to fix tears when they occur in young active patients. It is better to go through a rotator cuff repair with its accompanying 90% success rate in returning the patient to normal function and minimal to no pain, than to watch the shoulder worsen over time to become a painful crippled extremity.
In young patients who have massive tears that are scarred and retracted and unfixable, there are options but none are extraordinarily appetizing. Living with the shoulder is recommended for the patients who have unfixable tears and little to no pain. These patients likely have enough of the other three rotator cuff muscles still functioning that they can compensate for the unfixable torn one.
Occasionally, cortisone injections can take a painful weak arm and turn it into a painless weak arm that can be observed.
A muscle transfer such as the latissimus dorsi transfer is an option for the young patient with pain and weakness but no arthritis on x-rays. This surgery transfers a normal muscle to replace the irretrievable muscle. Since this procedure is performed infrequently, it is best performed at an academic center where the surgeon may perform a few annually opposed to the community where the surgeon may perform one every few years.
Other options in the young patient with an irreparable rotator cuff tear include a superior capsular reconstruction, arthroscopic debridement, and partial shoulder replacement surgery.
Many times patients with unfixable rotator cuff tears will have entrapments of the suprascapular nerve and releasing the nerve can offer these patients pain relief. Patients who have pain with palpation of the infraspinatus and supraspinatus (the two muscles innervated by the suprascapular nerve) or patients who have EMG (a nerve test) evidence of suprascapular entrapment are considered candidates for a nerve release.
For the patient with a massive unfixable painful rotator cuff tear who can not lift their arm (a condition called pseudo paralysis), options are particularly limited. This scenario is called rotator cuff arthropathy when it is accompanied by proximal migration of the humerus with respect to the glenoid. Arthritis is a component as the articular cartilage on the humeral head wears away as the humeral head rubs against the acromion above. Partial shoulder replacements (called humeral head replacements) may alleviate some of the pain but they do not improve the function of the shoulder. The only weapon in our armamentarium that can minimize pain and improve function is a reverse shoulder replacement, which is a wonderful option for the patient over the age of 65. These replacements are so new to shoulder surgery that many surgeons are not sure if they will last more than 15-20 years, which does not make them great options in the younger population where there still is not an answer for rotator cuff arthropathy.
Once the humerus has migrated superiorly, it is difficult for the deltoid to remain under tension and to lift the arm. Thus, people with rotator cuff arthropathy (rotator cuff tears and arthritis) will have pain, stiffness, crunching, and weakness with an inability to lift their arm. View Figure 6 & 7a. The reverse shoulder replacement pushes the humerus down. The restoration of the proper position of the humerus puts the deltoid under tension. The pain is relieved by the fact that the bones are no longer rubbing against each other, now replaced by metal rubbing against plastic. Function is improved by the fact that the deltoid is under tension and can now elevate the arm. View Figure 7b, 8 & 9.
Visit our YouTube channel for videos on this topic.
Definition:
Scapulothoracic bursitis
Symptoms:
Painful grinding/snapping sensation at the top corner of the shoulder blade.
Non-Operative Treatment:
Cortisone injection
Operative Treatment:
Exicsion of the bursa under the shoulder blade and the top corner of the scapula.
Recovery:
Sling for 3-4 weeks and physical therapy. Unrestricted activity is allowed at 8 weeks.
Diagnosis Tool
Use this as a guide to determine what could be wrong based on the symptoms exhibited. For example, if your symptom is mild pain, then the most likely diagnosis could be one of the following: 1. Impingement, 2. AC Joint Arthritis, or 5. Superior Laberal Tear (SLAP Tear).
Diagnosis
Impingement
AC Joint Arthritis
Glenohumeral Arthritis
Frozen Shoulder
Superior Labral Tear (SLAP Tear)
Anterior Labral Tear
Rotator Cuff Tear
Rotator Cuff Arthropathy
Calcific Tendinitis
Tumor
Disclaimer: By no means does this experimental diagnosis tool substitute for a physician’s opinion. It has NOT been validated as an accurate diagnosis maker and is only supplied for educational purposes to give a patient an idea of what symptoms could correspond to what diagnoses. It is strongly recommended that you seek formal medical advice from your physician instead of relying on this tool.